Objective: Since initial description by Forero for thoracic region, ultrasound guided erector spinae plane (ESP) block has experienced several surgeries for postoperative pain management, chronic pain or surgical anesthesia. Although ESP block has been reported to provide effective analgesia in the thoracic region, its effect in lumbar region still unclear. In this study we aimed to showed our successful experience with lumbar ESP block as a main anesthetic technique in fifteen high risk elderly patients undergoing hip surgery with mild propofol sedation.
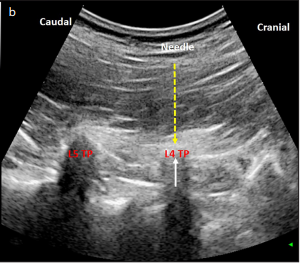
Materials and Methods: In this observational study high risk elderly fifteen patients received lumbar ESP block as a main anesthetic technique with mild propofol sedation. 40 mL of local anesthetic mixture (20 mL bupivacaine 0.5%, 10 mL lidocaine 2%, and 10 mL normal saline) was administered between the erector spinae muscles and transverse process at the level of the 4th lumbar vertebra. Also we demonstrate magnetic resonance images and discuss the anatomic basis of lumbar ESP block.
Results: All patients’ surgeries were completed without requirement for general anesthesia or local anesthesia infiltration of the surgical site. All patients’ pain scores were <2/10 in the recovery room. Significant contrast spread was observed between the Th12 and L5 transverse process and erector spinae muscle and between multifidus muscle and iliocostal muscle at the L2-4 levels. Contrast material was observed at the anterior of the transverse process spreading to the paravertebral, foraminal and partially epidural area/spaces and also in the areas where the lumbar nerves enter the psoas muscle.
Conclusion: Lumbar ESP block when combined with mild sedoanalgesia provides adequate and safe anesthesia in high risk elderly patients undergoing hip surgery.
Cite this article as: Ahiskalioglu A, Tulgar S, Celik M, Ozer Z, Alici HA, Aydin ME. Lumbar Erector Spinae Plane Block as a Main Anesthetic Method for Hip Surgery in High Risk Elderly Patients: Initial Experience with a Magnetic Resonance Imaging. Eurasian J Med 2020; 52(1): 16-20.

.png)
_In%20Progress-1%20(1)_page-0001.jpg)

.png)
.png)